
„Sme to, čo robíme opakovane. Dokonalosť potom nie je čin, ale zvyk.“
Aristotle, pretože toto citát môže byť nesprávne priradený, myšlienku, že konzistentnosť je pre úspech rozhodujúca, hlasne potvrdzujú okrem iného aj poprední športovci na svete, obchodné tykóny a Dr. Kristaps Jurj z Pauls Stradins Clinical University Hospital v Rige, Lotyšsko.
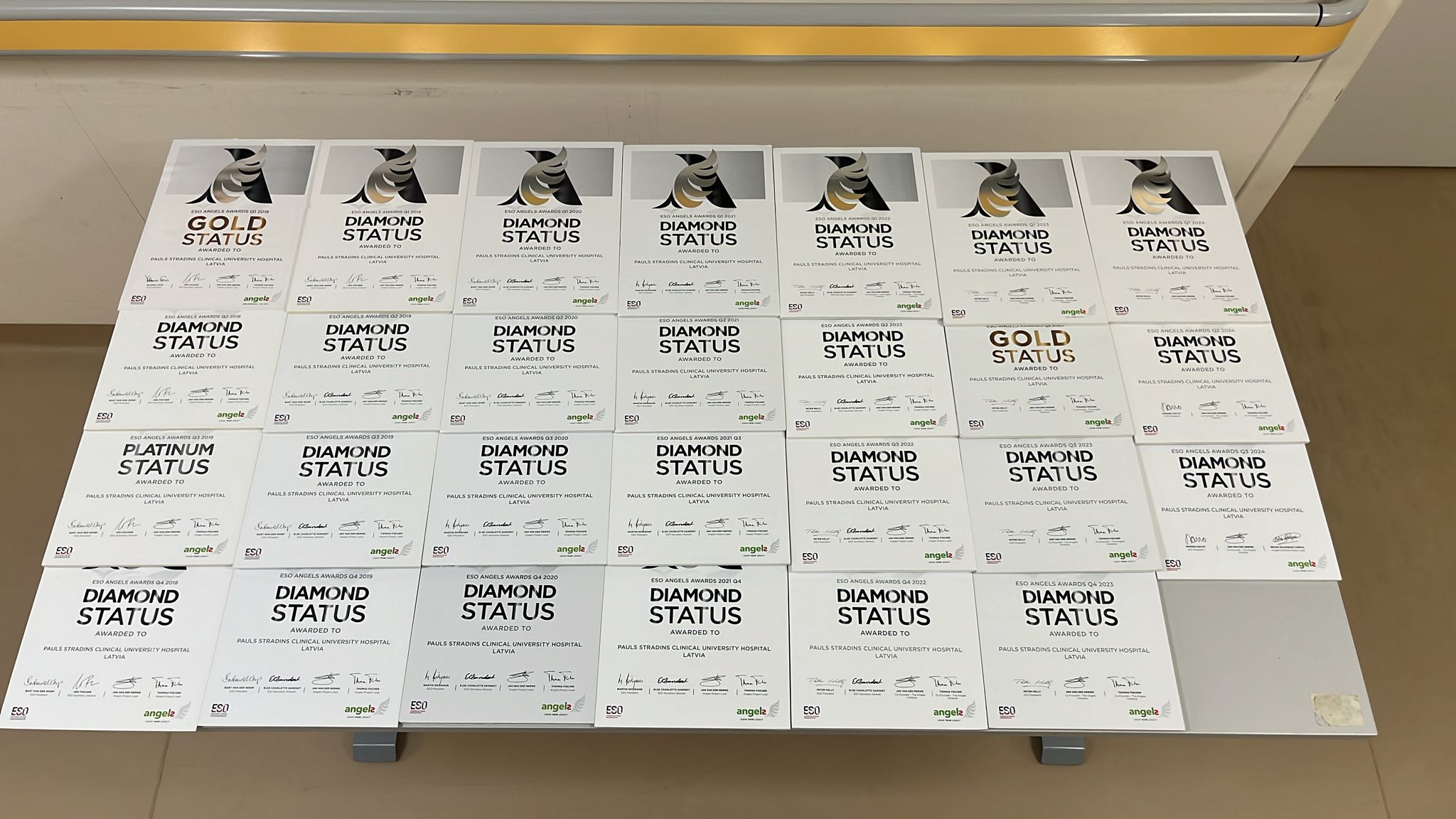
Ak by sa konala rebríčka pre ceny Angels Awards, nemocnica Dr. Jurja a 24 diamantových ocenení by bola hneď na vrchole a bez dohľadu. Prvýkrát sa dali do rúk na začiatku roku 2018, keď sa zaregistrovali v spoločnosti Angels, a do konca tohto roka začali horúcu sériu diamantových ocenení, ktoré by boli neprerušené, ale pre zmeškaný termín zadávania údajov v lete 2023.
„Niečo začnete, pracujte, kým si nemyslíte, že to funguje, a potom to stále robíte,“ vysvetľuje Dr. Jurjns. Keď dosiahnete konzistenciu, liečba akútnej cievnej mozgovej príhody sa stane „rutinou“ a ak je to rutina prvej triedy, potom „2-ročný klient môže urobiť správne rozhodnutie o liečbe za približne 10 minút“.
Dr. Jurj Pripisuje svoju sebadôveru tomu, že bol vyškolený najvýznamnejším apoplexiovým lekárom v lotyšskom a 2020 víťazom ESO Spirit of Excellence Award, prof. Evija Miglane. Ale pod jeho vedením prišiel apoplexiový tím v Pauls Stradins na medzinárodnú scénu a zostal tam. Počas podujatia Anjelská odborná príprava školiteľa, kde bol pozvaný ako prednášajúci, sa Dr. Jurj pripojil k publiku na prezentáciu poakútnej intervencie, projektu Arrow Project a videl ďalšiu príležitosť na zlepšenie.
Projekt Arrow, ktorý vyvinuli tri zdravotné sestry v Regionálnej univerzitnej nemocnici Málaga v Španielsku, štandardizuje starostlivosť po akútnej cievnej mozgovej príhode prostredníctvom systému farebne kódovaných šípok, ktoré pomáhajú lekárom, zdravotným sestrám a dokonca aj portérom ľahko identifikovať typ cievnej mozgovej príhody a postihnutej strany a prostredníctvom prístupových údajov QR kódu k liečebným protokolom pre každý deň, ako sú pravidelné kontroly dysfágie, glykémie a horúčky.
Dr. Jurj bol zasiahnutý jednoduchosťou a jasnosťou, ktorá je výsledkom použitia farieb a piktogramov vrátane tých, ktoré naznačujú, či bol pacient testovaný na problémy s prehĺtaním, a aké obmedzenia boli pri príjme potravy. V priebehu niekoľkých mesiacov sa prispôsobená verzia projektu zakorenila v jeho vlastnej jednotke mozgovej príhody.

Tu je niečo, čo by mohlo pomôcť
Prehĺtanie ľudí je zložitý obchod. Trvá to približne 50 párov svalov a niekoľko kraniálnych nervov, aby sa jedlo bezpečne prenieslo z lyžice do žalúdka – cesta pozostávajúca z troch fáz.
V orálnej fáze váš jazyk pozbiera jedlo a potom pracuje s čeľusťou, aby ho pohyboval po ústach pripravený na žuvanie. Žuvanie rozkladá jedlo na správnu veľkosť a textúru, pričom pomáha slinám, ktoré jedlo zmäkčujú.
V hltanovej fáze jazyk tlačí jedlo do zadnej časti úst, čím vyvoláva reakciu pri prehĺtaní, ktorá prechádza jedlom cez hrdlo. Aby sa zabránilo vniknutiu jedla alebo tekutiny do dýchacích ciest a pľúc, hlasová schránka sa tesne zatvára a dýchanie sa zastaví. Rozprávanie udržiava dýchacie cesty otvorené, čo môže byť dôvod, prečo vám matka povedala, aby ste počas jedenia nehovorili.
Pažeráková fáza trvá len približne tri sekundy, počas ktorých sa do pažeráka dostane jedlo alebo tekutina a prenesie sa do žalúdka.
Je to dobre koordinovaná svalová interakcia, na ktorú väčšina ľudí nikdy nemyslí, s výnimkou prípadov, keď niečo, čo jedia alebo pijú, „zlepší sa“. Potom kopa
alebo kašľový reflex sa zvyčajne pokúsi vyriešiť problém.
Ak však cievna mozgová príhoda alebo iná porucha nervového systému narúša reakciu na prehĺtanie, kusy jedla môžu zablokovať priechod vzduchu a jedlo alebo tekutina, ktorá zostáva v dýchacích cestách, sa môžu dostať do pľúc, čo vedie k aspiračnej pneumónii.
DrJurj bol znepokojený vysokým výskytom aspirácie v apoplexii, ktorá postihla až 30 percent pacientov. Tu je niečo, čo by mohlo pomôcť. Materiály preložil do lotyštiny a v auguste ich predstavil vo svojej nemocnici, pričom spolupracoval s výživovým a rečovým terapeutom, aby dodal viac podstaty smerniciam projektu Arrow.
Je príliš skoro na to, aby sme zmerali vplyv na rýchlosť aspirácie, ale existujú jasné opakujúce sa stránky vrátane skutočnosti, že zdravotné sestry sú teraz oprávnené hodnotiť pacientove schopnosti a spolu s výživovými špecialistami môžu namiesto toho, aby sa spoliehali na svoje praktické skúsenosti, postupovať podľa určitých spôsobov rozhodovania o diéte pacientov.
Piktogramy nie sú len nápomocné pre zdravotnícky personál. Pomáhajú tiež príbuzným pochopiť nutričné obmedzenia pacientov, hovorí Dr. Jurjns.
Jedným z problémov, ktoré sa snaží vyriešiť, je variabilita modifikovaných textúr (kategorizovaných ako nektár, med a puding), vďaka ktorým je jedlo bezpečné prehĺtať u pacientov v závislosti od ich skóre dysfágie. Aj tu bude kľúčom k úspechu dôslednosť.

„Uistite sa, že sa nezhorší“
Prvé stretnutie Dr. Jurja s pacientom s mozgovou mŕtvicou bolo prudkým požiarom v prvý alebo druhý deň jeho neurologického pobytu. Spomína si, že lekár, ktorý začal trombolýzu, bol odvolaný a nechal ho na starosti s pokynmi, aby pacienta pozoroval a robil si poznámky každých pätnásť minút. Nechala ho s desivou rozlúčkovou fotografiou: „Povedala, že sa nič nezhorší.“
Bol to úzkostný moment pre neurológa, ktorý sa v skutočnosti chcel stať ortopédom. Keď sa tento program ukázal ako plný, prekvapil svoju matku sledovaním jej krokov do neurológie. Majú rovnaké priezvisko a keď sa jej pacientka nedávno opýtala, či je spojená s „slávnym doktorom Jurjom“, prvý doktor Jurj úchytiek nebol úplne spokojný, hlási. (Bola nepochybne tiež hrdá.)
Stal sa špecialistom na mozgovú mŕtvicu z rovnakého dôvodu, ako chcel robiť ortopedické operácie – chcel si zašpiniť ruky a v neurológii sa mŕtvica dostala tam, kde bola akcia.
„Vždy je čo napraviť,“ hovorí Dr. Jurjns. Dokonca aj vtedy, keď musíte nechať niektoré svoje ocenenia v škatuliach, pretože stena displeja sa stala príliš malou. „Dochádza to pre mňa vo vlnách. Prichádza inšpirácia a potom urobím zmenu, urobím niečo nové.“
Niektoré z týchto zmien sa môžu javiť ako nevýznamné – napríklad piktogram na schránke alebo príručka Angelsova starostlivosť o mozgovú príhodu doma preložená do lotyštiny, aby sa zabránilo ašpirácii po prepustení – ale vykonávajú dôležitú prácu záchrany životov.
Na apoplexijnom úseku Regionálnej Univerzitnej nemocnice Málaga, kde sa do projektu Arrow vyvinula stručná norma ošetrovateľskej starostlivosti, prináša úspech aj konzistencia. Koncom roka 2023 vstúpili do tabuľky ocenení a práve získali druhú po sebe idúcu diamantovú cenu.
Je rozumné domnievať sa, že každá nemocnica, ktorá vyhrá diamanty v sérii, z dokonalosti stala návyk. Konzistentnosť sa počíta. A ak to budete robiť dostatočne dlho, nakoniec budete potrebovať väčšiu stenu.




